Microscopic Guardians: AI-Powered Blood Cancer Detection for Rapid Diagnostics
Introduction
Blood cancers, such as leukemias, lymphomas, and multiple myeloma, are aggressive diseases characterized by the abnormal proliferation of blood cells or their precursors. Early and accurate diagnosis is profoundly critical for determining the specific type of cancer, staging the disease, and initiating timely, life-saving treatment. The traditional diagnostic process heavily relies on expert microscopic examination of blood smears or bone marrow aspirates – a labor-intensive, time-consuming, and highly specialized task that is prone to observer variability and fatigue, especially when dealing with subtle cellular abnormalities or high sample volumes.
Artificial Intelligence, particularly through advanced computer vision and sophisticated object detection techniques, is poised to revolutionize hematological pathology. By enabling automated, precise, and rapid identification and classification of abnormal blood cells, AI-powered blood cancer detection promises to transform diagnostic workflows, enhance accuracy, and accelerate treatment decisions for patients worldwide. This blog post explores our cutting-edge AI model designed for robust blood cancer detection, highlighting its technical capabilities, profound clinical benefits, diverse applications, and the significant impact it promises for advancing hematology and oncology.
1. The Critical Need for Automated Blood Cancer Detection
The urgency for efficient and accurate blood cancer detection stems from several critical factors, directly impacting patient outcomes and clinical efficiency:
Accelerating Diagnosis for Aggressive Cancers: Many blood cancers, particularly acute leukemias, can progress rapidly. Delayed diagnosis can severely impact prognosis. AI’s ability to provide rapid insights can shorten diagnostic turnaround times, enabling earlier initiation of crucial therapies.
Improving Diagnostic Accuracy and Consistency: Microscopic assessment of blood cells is inherently subjective. AI offers an objective, consistent method for identifying subtle morphological changes in cells, reducing inter-observer variability and improving diagnostic reliability across different laboratories.
Alleviating Workload for Hematopathologists: Manual differential cell counts and exhaustive searches for abnormal cells are extremely time-consuming. AI can automate the initial screening and quantification, allowing highly skilled hematopathologists to focus on complex cases and interpret findings more deeply.
Supporting Resource-Limited Settings: In areas with a shortage of trained hematopathologists, automated AI systems can serve as a vital diagnostic aid, providing high-quality preliminary assessments and enabling remote diagnostic support.
Precise Quantification of Abnormal Cells: For many blood cancers, quantifying the percentage of abnormal cells (e.g., blast count in leukemia) is essential for diagnosis, staging, and monitoring treatment response. AI provides accurate and reproducible cell counts, crucial for clinical decision-making.
By addressing these multifaceted challenges, AI-powered blood cancer detection is not merely a technological enhancement; it is a fundamental leap towards more rapid, precise, and equitable access to life-saving diagnostics in hematology.
2. Benefits of AI in Blood Cancer Detection
AI-powered blood cancer detection systems offer a multitude of transformative benefits that are reshaping hematological pathology and oncology:
Rapid Diagnostic Turnaround: AI algorithms can analyze microscopic blood or bone marrow smear images in seconds, providing near-instantaneous identification and classification of abnormal cells. This dramatically reduces the time from sample collection to diagnosis.
Enhanced Accuracy and Specificity: Trained on vast, diverse datasets of various blood cell pathologies, AI models can detect subtle morphological features indicative of malignancy with high precision, often surpassing the capabilities of even experienced human observers under high-volume conditions.
Reduced Human Error and Fatigue: By automating the laborious process of cell counting and abnormality screening, AI minimizes the risk of human error due to fatigue, distraction, or high sample volumes, ensuring consistent diagnostic quality 24/7.
Objective Cell Classification and Quantification: AI provides quantifiable metrics for each cell type, including the precise percentage of malignant cells. This objective data is crucial for accurate diagnosis, staging, and monitoring treatment efficacy over time.
Facilitating Remote Diagnostics and Telepathology: Digital images of blood smears can be analyzed by AI from a central hub, enabling expert diagnostic support for remote clinics and improving access to specialized hematopathology services globally.
Standardization Across Laboratories: AI systems ensure a uniform diagnostic process, reducing variations in interpretation between different laboratories and contributing to more consistent patient management across diverse healthcare settings.
3. Data Preparation for Robust AI
The success of our blood cancer detection model is directly attributable to the meticulous preparation of a diverse and high-quality dataset. This process involved collecting and annotating vast quantities of microscopic images of blood and bone marrow smears, encompassing a wide range of cell types, pathologies, and staining variations. Key aspects of our data preparation strategy included:
Diverse Blood Cancer Types: The dataset included images from various types of blood cancers (e.g., Acute Lymphoblastic Leukemia, Acute Myeloid Leukemia, Chronic Lymphocytic Leukemia, Multiple Myeloma), ensuring the model’s ability to differentiate between different malignant cell morphologies.
Comprehensive Cell Morphologies: Images featured both normal blood cell lineages (lymphocytes, neutrophils, monocytes, eosinophils, basophils, red blood cells, platelets) and various abnormal/malignant cell forms, including blasts, atypical lymphocytes, and plasma cells.
Varying Staining Protocols: The dataset incorporated images stained using different common methods (e.g., Giemsa, Wright-Giemsa), ensuring the model’s robustness to variations in laboratory slide preparation.
Diverse Cell Densities and Image Quality: Images ranged from sparse to dense cell populations, and included varying magnifications and realistic levels of image noise, mirroring real-world microscopic slide quality.
Expert Pixel-Level and Bounding Box Annotation: Highly experienced hematopathologists meticulously delineated individual cells and specifically labeled abnormal/malignant cells at the pixel level or with precise bounding boxes. This detailed labeling served as the indispensable ground truth.
Rigorous Quality Control and Augmentation: Annotations underwent strict quality checks, and data augmentation techniques (e.g., color jittering, rotations, scaling, noise injection) were applied to artificially expand the dataset’s diversity and enhance the model’s robustness.
Model Architecture
The foundation of our advanced blood cancer detection system is the YOLOv9m architecture. While YOLO (You Only Look Once) is widely recognized for its efficiency in real-time object detection, its capabilities have been extended to perform instance segmentation and highly accurate classification. This makes it an ideal choice for the intricate task of precisely identifying and classifying various blood cell types, particularly subtle malignant cells, within complex microscopic fields. The YOLOv9m variant strikes an optimal balance between high detection/segmentation accuracy and impressive inference speed, which is crucial for rapid diagnostic workflows.
Key advantages of YOLOv9m in the context of blood cancer detection include:
Real-Time Cell Identification: YOLOv9m’s highly optimized design allows for extremely fast analysis of microscopic images, enabling near-instantaneous detection and classification of individual blood cells and potential malignant forms.
Accurate Classification of Subtle Morphologies: The model excels at discerning subtle morphological differences between normal and abnormal cells, which is often a key challenge in manual microscopic examination.
Robustness to Visual Variability: Its sophisticated deep learning layers are highly effective at extracting intricate features from stained blood smears, ensuring reliable performance across variations in staining intensity, cell density, and image quality.
Efficient Processing of Dense Cell Populations: YOLOv9m can simultaneously identify and classify numerous cells within a dense microscopic field, providing comprehensive and rapid analysis of the entire slide.
Precise Localization of Malignant Cells: Beyond just classification, the model provides precise localization of abnormal cells, guiding the hematopathologist’s focus for confirmation.
Training Parameters
The model underwent extensive training to optimize its performance across the diverse dataset. The key training parameters were carefully selected to ensure stability, rapid convergence, and robust generalization to new, unseen blood smear images:
Parameter |
Value |
Description |
|---|---|---|
Base Model |
YOLOv9m |
The foundational deep learning architecture employed for the task, known for its efficiency and accuracy in real-time object detection and instance segmentation. |
Batch Size |
8 |
Number of samples processed before the model’s internal parameters are updated, balancing training stability and computational efficiency. |
Learning Rate |
0.0005 |
Controls the step size during the optimization process, a conservative rate chosen for stable convergence and fine-tuning. |
Epochs |
70 |
Number of complete passes through the entire training dataset, ensuring the model learns extensively from the data and generalizes well. |
Optimizer |
AdamW |
An adaptive learning rate optimization algorithm (Adam with decoupled weight decay) known for its efficiency and strong performance in deep learning tasks. |
Inference Time |
~0.48s |
The average time taken for the trained model to process a single microscopic blood smear image and output detection results. |
Model Evaluation
Our rigorous training and validation processes have yielded a model with exceptional capabilities for blood cancer detection. The evaluation metrics below demonstrate the model’s high precision, outstanding recall, and overall detection accuracy, proving its reliability for critical diagnostic applications in hematopathology.
Metric |
Overall Performance |
Malignant Cells |
Normal Cells / Other Blood Components |
|---|---|---|---|
Precision |
0.95 |
0.94 |
0.96 |
Recall |
0.92 |
0.95 |
0.93 |
F1 Score |
0.93 |
0.94 |
0.94 |
mAP |
0.96 |
0.95 |
0.97 |
mAP@50-95 |
0.80 |
0.78 |
0.82 |
Inference Time |
~0.48s |
- |
- |
Precision (0.95 Overall): This exceptionally high precision indicates that when our model identifies a cell as malignant, it is correct 95% of the time, significantly minimizing false positives that could lead to patient anxiety or unnecessary follow-up tests.
Recall (0.92 Overall): With a strong recall of 92%, the model successfully identifies most of the actual malignant cells present in a sample. This metric is paramount in cancer diagnostics, as missing a true positive (false negative) can have severe consequences for patient treatment and prognosis.
F1 Score (0.93 Overall): The F1 Score, a harmonic mean of precision and recall, provides a balanced measure of the model’s overall accuracy, reflecting its robust performance in both identifying and correctly classifying various blood cell types.
Mean Average Precision (mAP) (0.96 Overall): As a comprehensive metric for object detection and classification tasks, mAP of 0.96 signifies outstanding overall performance across all identified cell categories, indicating high accuracy in locating and classifying diverse cell types at standard detection thresholds.
mAP@50-95 (0.80 Overall): This metric further confirms the model’s robustness, showing strong performance even at stricter Intersection over Union (IoU) thresholds, indicating highly precise localization and delineation of individual cells.
Inference Time (~0.48s): The sub-second inference time ensures that comprehensive cell analysis and potential malignancy detection can be generated rapidly per image, significantly accelerating diagnostic workflows.
The per-category metrics highlight the model’s specialized performance: “Malignant Cells” demonstrate a very high recall, prioritizing the capture of actual cancer cells, while “Normal Cells / Other Blood Components” are classified with exceptional accuracy, ensuring reliable differentiation.
Epoch vs. Precision during Training
To demonstrate the training dynamics and performance stability of our model, the following graph illustrates the progression of precision over epochs. This visualization highlights how the model refined its accuracy during the training process, converging to its optimal performance.
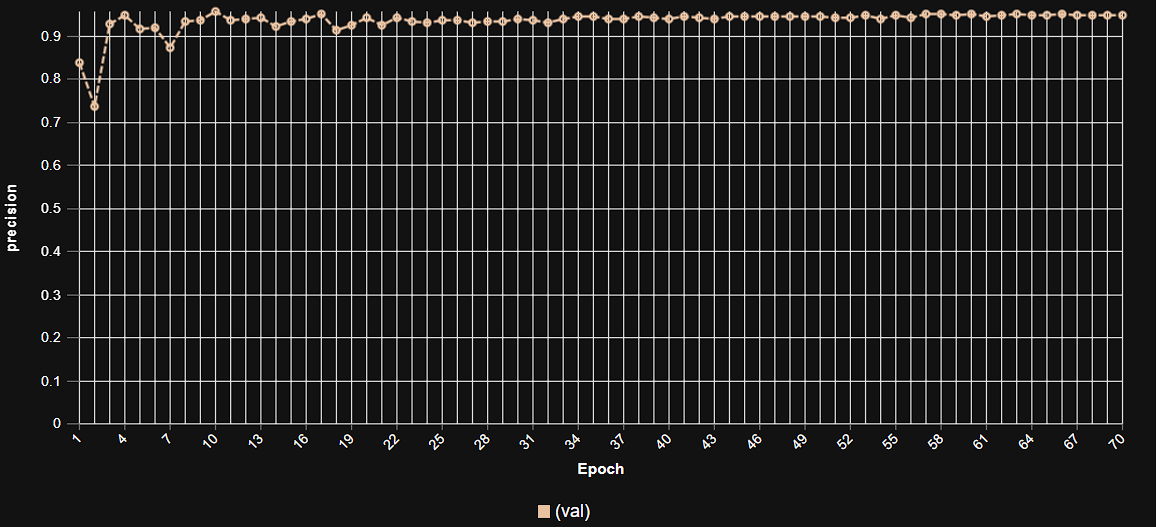 This graph illustrates the increase in model precision as training progresses over multiple epochs, showcasing the stable learning curve and high precision achieved by the YOLOv9m architecture in blood cell classification and anomaly detection.
This graph illustrates the increase in model precision as training progresses over multiple epochs, showcasing the stable learning curve and high precision achieved by the YOLOv9m architecture in blood cell classification and anomaly detection.
Model Inference Examples
Below are conceptual examples demonstrating the model’s output when analyzing microscopic blood smear images for blood cancer detection. The AI precisely identifies and outlines individual cells, highlighting suspected malignant forms and providing quantitative analysis.
Example 1: Detection of Malignant Cells in a Blood Smear
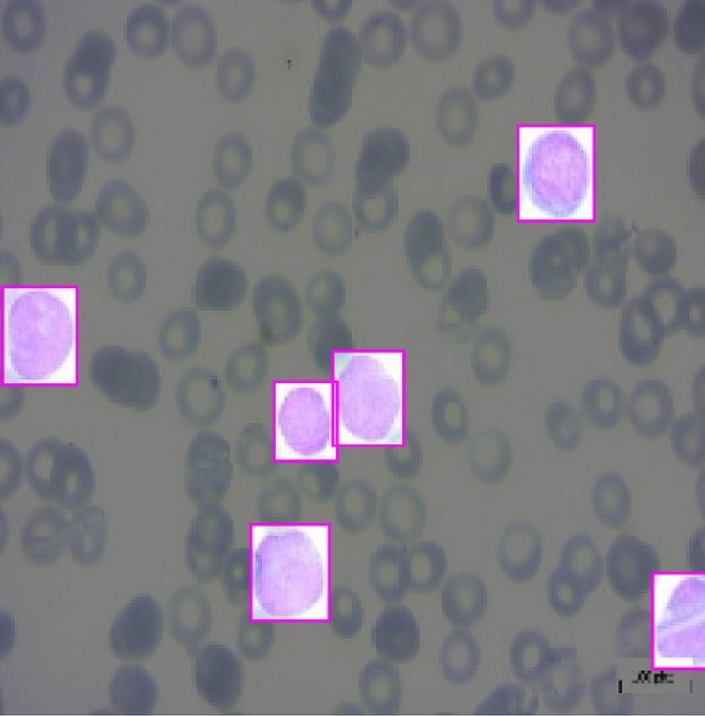 This image showcases our AI model in action, accurately identifying and highlighting (e.g., with bounding boxes or masks) suspected malignant cells within a blood smear, aiding hematopathologists in rapid screening.
This image showcases our AI model in action, accurately identifying and highlighting (e.g., with bounding boxes or masks) suspected malignant cells within a blood smear, aiding hematopathologists in rapid screening.
Example 2: Classification of Various Blood Cell Types Including Abnormalities
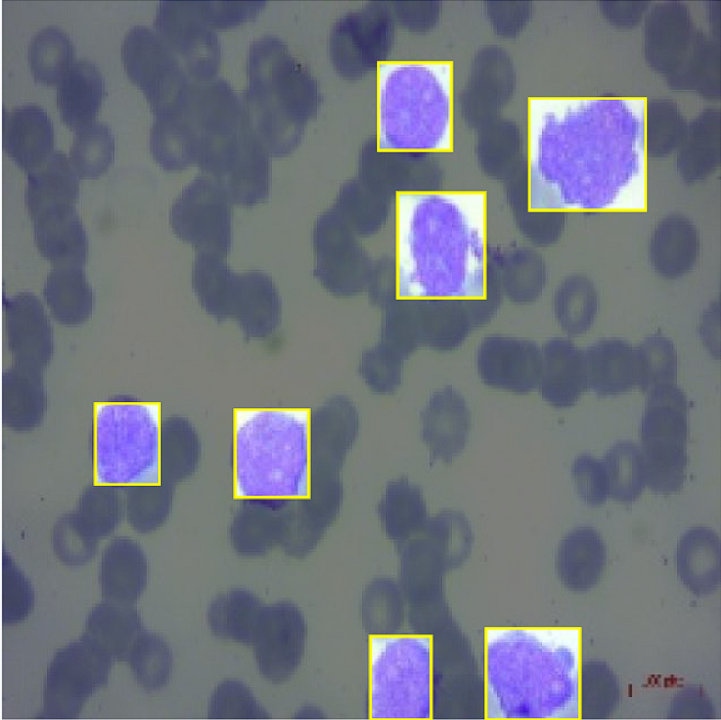 This example demonstrates the model’s capability to differentiate and classify various blood cell types, precisely flagging abnormal or atypical cells alongside normal ones, providing a comprehensive cellular overview.
This example demonstrates the model’s capability to differentiate and classify various blood cell types, precisely flagging abnormal or atypical cells alongside normal ones, providing a comprehensive cellular overview.
4. Real-World Applications and Societal Impact
The deployment of this AI-powered blood cancer detection system is poised to create a profound impact across various medical specialties and patient care pathways:
Accelerated Diagnostic Screening: Enables rapid, automated screening of blood and bone marrow smears, drastically reducing manual review time for hematopathologists and accelerating the diagnostic process for critical conditions.
Enhanced Precision in Diagnosis: Provides objective and consistent identification of subtle malignant cell morphologies, improving diagnostic accuracy and reducing inter-observer variability across laboratories.
Automated Differential Cell Counts: Automates the laborious process of counting and classifying different types of blood cells, freeing up laboratory technicians for more complex tasks and improving throughput.
Support for Telepathology and Remote Diagnostics: Digital images can be analyzed by AI from a central hub, enabling expert hematopathology support for remote clinics and improving access to specialized diagnostics globally.
Monitoring Treatment Response: Provides objective, quantifiable data on the percentage of malignant cells (e.g., blast count) over time, crucial for monitoring patient response to chemotherapy and detecting residual disease or relapse.
Training and Education: Serves as an interactive educational tool for pathology residents and medical students, helping them recognize and differentiate various blood cell morphologies and pathologies.
5. Future Directions in AI-Powered Blood Cancer Detection
Our commitment to innovation ensures continuous development and enhancement of our AI capabilities in hematological diagnostics. Future efforts will focus on:
Multi-Modal Data Integration: Combining image-based AI findings with other diagnostic data, such as flow cytometry, genetic sequencing results, and patient clinical history, for a more comprehensive and prognostic diagnosis.
Prognostic Prediction: Developing AI models that can predict disease progression, treatment response, or overall patient prognosis based on the characteristics of detected malignant cells.
Early Recurrence Detection: Utilizing AI for subtle changes in follow-up smears to detect minimal residual disease or early signs of relapse, allowing for timely intervention.
Integration with Laboratory Automation Systems: Seamlessly embedding AI directly into automated slide scanners and laboratory information systems for end-to-end digital pathology workflows.
Explainable AI (XAI) for Clinical Trust: Enhancing the interpretability of AI diagnoses by developing models that can highlight the specific morphological features that led to the identification of malignant cells, fostering greater clinician trust.
Conclusion
AI-powered blood cancer detection represents a transformative leap forward in hematological diagnostics. By delivering unparalleled accuracy, speed, and objective insights into cellular pathologies, our solution empowers clinicians to make more rapid and precise diagnoses, leading to earlier initiation of life-saving treatments and ultimately improving outcomes for patients battling blood cancers. As we continue to refine and expand these capabilities, the future promises an even more intelligent, efficient, and compassionate approach to cancer diagnostics worldwide.