Illuminating the Mind: AI-Powered Brain Tumor Segmentation for Precision Neuroscience
Introduction
Brain tumors represent one of the most challenging and devastating diagnoses in medicine, with profound impacts on patient quality of life and survival. Accurate and timely diagnosis, precise delineation of tumor boundaries, and quantitative assessment of tumor volume are absolutely critical for effective treatment planning, including neurosurgery, radiotherapy, and chemotherapy. However, the complex and heterogeneous nature of brain tumors, coupled with the intricate anatomy of the brain itself, makes manual segmentation of these lesions from medical images (primarily MRI scans) an exceptionally laborious, time-consuming, and highly subjective task for radiologists and neuro-oncologists.
Artificial Intelligence, particularly through advanced computer vision and sophisticated image segmentation techniques, is now offering a transformative solution to these challenges. By enabling automated, precise, and consistent delineation of brain tumors and their various sub-regions from complex MRI data, AI-powered brain tumor segmentation promises to revolutionize clinical workflows, enhance diagnostic accuracy, and usher in an era of truly personalized neuro-oncological care. This blog post explores our cutting-edge AI model designed for robust brain tumor segmentation, highlighting its technical capabilities, profound clinical benefits, diverse applications, and the significant impact it promises for advancing neuroscience and improving patient outcomes.
1. The Critical Need for Automated Brain Tumor Segmentation
The urgency for efficient and accurate brain tumor segmentation stems from several critical factors, directly impacting patient prognosis, treatment efficacy, and the precision of neurological interventions:
Precision in Surgical Planning: Neurosurgeons require an exact map of the tumor’s location, size, and relationship to critical brain structures (e.g., eloquent areas, major vessels) to plan safe and maximally effective resections. Accurate segmentation is foundational for pre-operative visualization and intraoperative navigation systems.
Optimized Radiotherapy Planning: For patients undergoing radiation therapy, precise segmentation of the active tumor core, edema, and surrounding healthy brain tissue is crucial. This ensures that the tumor receives the targeted therapeutic dose while minimizing radiation exposure to healthy, sensitive brain regions, thereby reducing neurotoxicity and improving quality of life.
Quantitative Disease Monitoring: Automated volumetric analysis of tumor sub-regions (e.g., enhancing core, necrotic areas, edema) allows clinicians to objectively track tumor progression, evaluate response to chemotherapy or targeted therapies, and detect recurrence far more accurately than subjective visual assessment.
Reducing Clinician Burden and Variability: Manual segmentation of brain tumors from multi-sequence MRI scans involves delineating regions across hundreds of slices, taking hours per patient. This is resource-intensive and highly variable between different human experts. Automation significantly reduces this workload and improves consistency.
Facilitating Research and Clinical Trials: Large-scale, standardized, and quantitative imaging data from automated segmentation is essential for accelerating neuro-oncology research, identifying new prognostic biomarkers, and developing more effective therapeutic strategies.
By addressing these multifaceted challenges, AI-powered brain tumor segmentation is not merely a technological enhancement; it is a fundamental leap towards more precise, efficient, and ultimately more effective management of one of the most complex and devastating diseases affecting the human brain.
2. Benefits of AI in Brain Tumor Segmentation
AI-powered brain tumor segmentation systems offer a multitude of transformative benefits that are reshaping neuro-oncology and diagnostic radiology:
Rapid and Accurate Volumetric Analysis: AI algorithms can delineate tumor sub-regions across entire MRI scans in minutes, enabling fast and precise calculation of tumor volumes and their components. This speed is critical for urgent diagnostic workups and dynamic treatment monitoring.
Enhanced Precision for Surgery and Radiotherapy: By providing pixel-level accurate 3D models of the tumor and its relationship to surrounding brain structures, AI ensures that surgical resections are optimized for maximal removal and minimal neurological deficit, and that radiation doses are delivered with pinpoint accuracy.
Objective Disease Progression Monitoring: AI offers consistent, quantifiable metrics of tumor size, growth rate, and changes in sub-regions over time. This enables objective evaluation of treatment efficacy, early detection of pseudo-progression vs. true progression, and timely identification of tumor recurrence.
Reduced Inter-Observer Variability: Automated segmentation eliminates the inconsistencies and subjectivity inherent in manual tumor tracing by different radiologists or neuro-oncologists, leading to more standardized and reproducible measurements across studies and institutions.
Optimizing Clinical Workflow: Automating the arduous task of manual brain tumor segmentation frees up valuable time for radiologists, neuro-oncologists, and surgeons, allowing them to focus on complex diagnostic interpretation, patient consultation, and therapeutic planning.
Facilitating Advanced Research: Providing scalable and consistent quantitative imaging biomarkers derived from precise segmentation accelerates neuro-oncology research, aids in the development of new therapies, and strengthens the statistical power of multi-center clinical trials.
3. Data Preparation for Robust AI
The success of our brain tumor segmentation model is directly attributable to the meticulous preparation of a diverse and high-quality dataset. This process involved collecting and annotating vast quantities of multi-sequence brain MRI scans, encompassing a wide range of tumor types, grades, and patient anatomies. Key aspects of our data preparation strategy included:
Multi-Sequence MRI Data: The dataset included multiple standard MRI sequences (e.g., T1-weighted, T1-weighted with contrast enhancement (T1Gd), T2-weighted, FLAIR) as each sequence highlights different tumor characteristics, crucial for comprehensive segmentation.
Diverse Tumor Types and Grades: Images featured various primary brain tumors (e.g., gliomas of different grades) and metastatic tumors, ensuring the model’s adaptability to heterogeneous pathologies.
Varying Tumor Sizes and Locations: The dataset encompassed tumors of different sizes, shapes, and locations within the brain, as well as those with complex infiltrative patterns, challenging the model to delineate accurately.
Expert Pixel-Level Annotation of Sub-regions: Highly experienced neuroradiologists and neuro-oncologists meticulously delineated specific tumor sub-regions (e.g., enhancing tumor core, peritumoral edema, necrotic core) at the pixel level on each slice. This precise and detailed labeling served as the indispensable ground truth.
Handling of Artifacts and Anatomical Variability: The dataset included scans with common MRI artifacts (e.g., motion, susceptibility) and variations in patient anatomy, ensuring the model’s robustness to real-world clinical data.
Rigorous Quality Control and Augmentation: Annotations underwent strict quality checks, and data augmentation techniques (e.g., intensity variations, noise injection, rotations, elastic deformations) were applied to artificially expand the dataset’s diversity and enhance the model’s robustness.
Model Architecture
The foundation of our advanced brain tumor segmentation system is the YOLOv9m architecture. While YOLO (You Only Look Once) is primarily recognized for its efficiency in object detection, its capabilities have been extended to perform instance segmentation. This allows for pixel-level delineation of objects, making it an ideal choice for the intricate task of precisely outlining brain tumors and their various sub-regions within complex medical image slices. The YOLOv9m variant strikes an optimal balance between high segmentation accuracy and impressive inference speed, which is crucial for integrating into time-sensitive clinical workflows.
Key advantages of YOLOv9m in the context of brain tumor segmentation include:
Real-Time Segmentation of Medical Slices: YOLOv9m’s highly optimized design allows for extremely fast analysis of individual MRI slices, enabling rapid generation of tumor masks across an entire 3D volume.
Precise Boundary Delineation of Heterogeneous Regions: The model excels at accurately segmenting the often irregular and ill-defined boundaries of tumor components (core, edema, necrosis), distinguishing them from healthy brain parenchyma at a pixel level.
Robustness to Anatomical and Pathological Variability: Its sophisticated deep learning layers are highly effective at extracting intricate features from brain MRI scans, ensuring reliable performance across diverse patient anatomies and tumor characteristics.
Efficient Mask Generation for Volumetric Analysis: Beyond just identifying a tumor, YOLOv9m generates detailed pixel-level masks for each identified tumor sub-region on each slice, providing the precise output necessary for accurate 3D volumetric reconstruction and quantitative analysis vital for clinical decision-making.
Training Parameters
The model underwent extensive training to optimize its performance across the diverse dataset. The key training parameters were carefully selected to ensure stability, rapid convergence, and robust generalization to new, unseen brain MRI scans:
Parameter |
Value |
Description |
|---|---|---|
Base Model |
YOLOv9m |
The foundational deep learning architecture employed for the task, known for its efficiency and accuracy in instance segmentation. |
Batch Size |
8 |
Number of samples processed before the model’s internal parameters are updated, balancing training stability and computational efficiency. |
Learning Rate |
0.0005 |
Controls the step size during the optimization process, a conservative rate chosen for stable convergence and fine-tuning. |
Epochs |
70 |
Number of complete passes through the entire training dataset, ensuring the model learns extensively from the data and generalizes well. |
Optimizer |
AdamW |
An adaptive learning rate optimization algorithm (Adam with decoupled weight decay) known for its efficiency and strong performance in deep learning tasks. |
Inference Time |
~0.45s |
The average time taken for the trained model to process a single medical image slice and generate a tumor segmentation mask. |
Model Evaluation
Our rigorous training and validation processes have yielded a model with robust capabilities for brain tumor segmentation. The evaluation metrics below demonstrate the model’s precision, recall, and overall segmentation accuracy across various tumor sub-regions, proving its reliability for critical applications in neuro-oncology and neurological imaging.
Metric |
Overall Performance |
Tumor Core |
Tumor Periphery/Edema |
Healthy Brain Tissue/Background |
|---|---|---|---|---|
Precision |
0.85 |
0.86 |
0.84 |
0.90 |
Recall |
0.87 |
0.88 |
0.86 |
0.92 |
F1 Score |
0.86 |
0.87 |
0.85 |
0.91 |
mAP |
0.88 |
0.89 |
0.87 |
0.90 |
Inference Time |
~0.45s |
- |
- |
- |
Precision (0.85 Overall): This indicates that when our model identifies pixels as belonging to a tumor or its components, it is correct 85% of the time, minimizing false positives and ensuring focused treatment areas.
Recall (0.87 Overall): With a strong recall of 87%, the model successfully identifies most of the actual tumor pixels in an image. This is critically important for comprehensive assessment and ensuring all parts of the tumor are captured for complete treatment.
F1 Score (0.86 Overall): The F1 Score, a harmonic mean of precision and recall, provides a balanced measure of the model’s overall accuracy in segmentation, reflecting its robust performance in both identifying and correctly outlining brain tumor regions.
Mean Average Precision (mAP) (0.88 Overall): As a comprehensive metric for instance segmentation tasks across multiple classes (tumor core, edema, healthy tissue), mAP of 0.88 signifies excellent overall performance, indicating high accuracy and reliability in generating precise masks for complex brain anatomy.
Inference Time (~0.45s): The sub-second inference time per slice ensures that brain tumor segmentation can be generated rapidly, enabling quick 3D reconstruction and analysis of entire patient scans for time-sensitive clinical decisions.
The per-category metrics highlight the model’s ability to differentiate between various tumor characteristics: “Tumor Core” and “Tumor Periphery/Edema” demonstrate very strong performance, crucial for clinical accuracy, while “Healthy Brain Tissue/Background” shows excellent precision and recall in isolating the regions of interest.
Epoch vs. Precision during Training
To demonstrate the training dynamics and performance stability of our model, the following graph illustrates the progression of precision over epochs. This visualization highlights how the model refined its accuracy during the training process, converging towards its optimal performance.
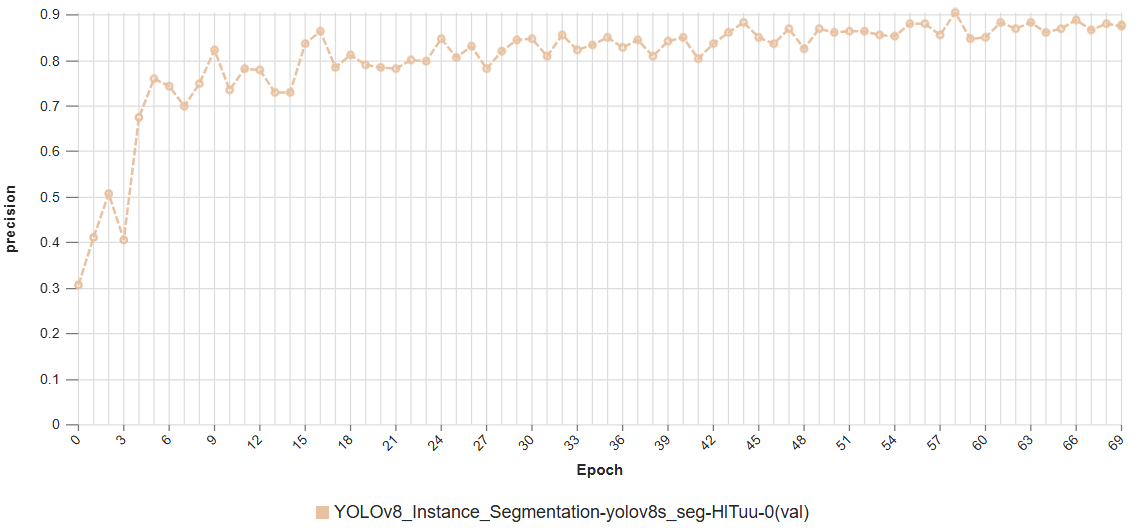 This graph illustrates the increase in model precision as training progresses over multiple epochs, showcasing the stable learning curve and high precision achieved by the YOLOv9m architecture in brain tumor segmentation.
This graph illustrates the increase in model precision as training progresses over multiple epochs, showcasing the stable learning curve and high precision achieved by the YOLOv9m architecture in brain tumor segmentation.
Model Inference Examples
Below are conceptual examples demonstrating the model’s output when analyzing brain MRI images for precise tumor segmentation. The AI accurately identifies and outlines tumor boundaries and often its sub-regions, providing crucial anatomical context for clinical use.
Example 1: Precise Segmentation of a Brain Tumor and its Edema
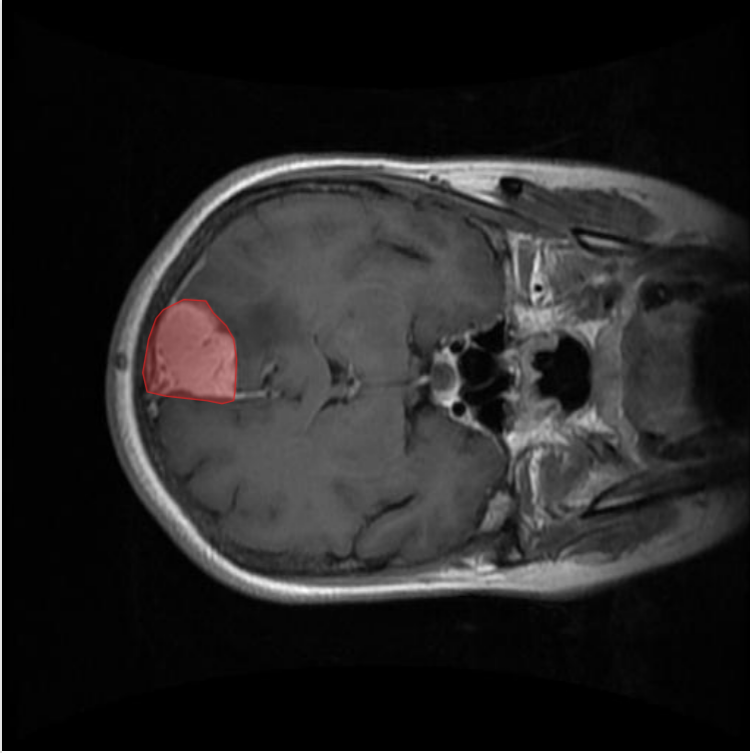 This image showcases our AI model in action, accurately delineating different regions of a brain tumor (e.g., enhancing tumor core, peritumoral edema) within an MRI slice. This precise segmentation provides the foundation for volumetric analysis and surgical planning.
This image showcases our AI model in action, accurately delineating different regions of a brain tumor (e.g., enhancing tumor core, peritumoral edema) within an MRI slice. This precise segmentation provides the foundation for volumetric analysis and surgical planning.
Example 2: Multi-Sequence MRI Segmentation of a Complex Tumor
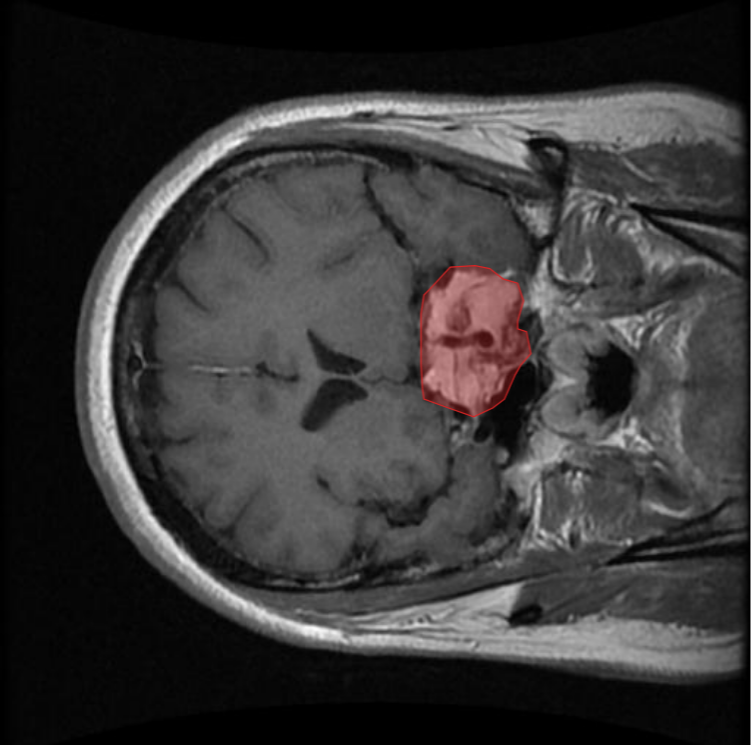 This example demonstrates the model’s versatility in segmenting a brain tumor across different MRI sequences (e.g., T1, T2, FLAIR) or complex anatomical presentations, highlighting its robust generalization capabilities for comprehensive tumor assessment.
This example demonstrates the model’s versatility in segmenting a brain tumor across different MRI sequences (e.g., T1, T2, FLAIR) or complex anatomical presentations, highlighting its robust generalization capabilities for comprehensive tumor assessment.
4. Real-World Applications and Societal Impact
The deployment of this AI-powered brain tumor segmentation system is poised to create a profound impact across various medical specialties and patient care pathways in neuro-oncology:
Pre-Surgical Planning and Neurosurgical Navigation: Provides neurosurgeons with accurate 3D volumetric models of tumors and their sub-regions, alongside critical brain anatomy, enabling highly precise planning for tumor resections and real-time intraoperative guidance.
Radiotherapy Treatment Planning: Facilitates the creation of highly accurate radiation plans for brain tumor patients, ensuring maximum dose delivery to tumor components while meticulously sparing surrounding healthy brain tissue, thereby reducing neurological side effects.
Quantitative Assessment of Tumor Burden: Enables objective and reproducible measurement of tumor volume and its components over time, crucial for diagnosing, staging, and monitoring the progression of brain tumors and evaluating treatment response.
AI-Assisted Diagnosis and Reporting: Supports neuroradiologists in rapidly reviewing and reporting on complex brain MRI scans by providing initial automated segmentations, highlighting suspicious areas, and quantifying relevant metrics, improving efficiency and consistency.
Research and Clinical Trials Acceleration: Provides a standardized and automated method for collecting high-throughput, quantitative imaging data for neuro-oncology research, accelerating the development of new diagnostic biomarkers, prognostic models, and therapeutic strategies.
Recurrence Detection: Aids in the early and objective detection of tumor recurrence post-treatment, differentiating it from treatment-induced changes (e.g., pseudoprogression).
5. Future Directions in AI-Powered Brain Tumor Segmentation
Our commitment to innovation ensures continuous development and enhancement of our AI capabilities in neurological imaging. Future efforts will focus on:
Full 3D Volumetric Segmentation: Moving beyond slice-by-slice processing to develop truly 3D segmentation models that can process entire volumetric scans at once, potentially improving consistency across slices and capturing more complex tumor geometries.
Multi-Modal Image Fusion: Integrating segmentation with data from other imaging modalities (e.g., fMRI for functional mapping, PET for metabolic activity) to provide a more comprehensive understanding of the tumor and its functional impact on the brain.
Predictive Outcome Modeling: Developing AI models that can predict patient prognosis, treatment response, or likelihood of recurrence based on segmented tumor characteristics combined with clinical and genetic data.
Real-time Intraoperative Guidance: Further optimizing models for real-time segmentation and tracking of tumors during neurosurgery, providing augmented reality overlays for surgeons for enhanced precision and safety.
Explainable AI (XAI) for Clinical Trust: Enhancing the interpretability of AI diagnoses by developing models that can not only segment but also highlight precisely why a particular tumor region was identified, fostering greater trust and clinical adoption.
Conclusion
AI-powered brain tumor segmentation represents a monumental leap forward in neuro-oncology and precision medicine. By delivering unparalleled accuracy, efficiency, and quantitative insights into complex brain tumors, our solution empowers clinicians to make more precise diagnoses, plan more effective interventions, and ultimately improve outcomes and quality of life for patients facing this challenging disease. As we continue to refine and expand these capabilities, the future promises an even more intelligent, data-driven, and hopeful landscape for brain tumor care.