Eye Disease Detection in Retinal Images: Advancing Ophthalmic Care with AI
Introduction
Artificial Intelligence is rapidly transforming the healthcare landscape by introducing unprecedented efficiencies and diagnostic capabilities. Eye diseases represent a significant global health burden, affecting hundreds of millions of people worldwide and leading to preventable vision impairment and blindness if left undetected or untreated. The traditional diagnostic workflow for eye conditions often relies on specialized equipment and the expertise of ophthalmologists, which can lead to accessibility challenges in underserved areas and delays in diagnosis due to high patient volumes.
This blog post explores the application of AI in detecting eye diseases from retinal images, focusing on a model trained to identify cataract, glaucoma, diabetic retinopathy, and normal eye conditions. By integrating state-of-the-art AI into clinical practice, we are not just identifying diseases; we are actively preventing vision loss and significantly improving global eye health outcomes.
1. Why Eye Disease Detection Matters
The ability to accurately and timely diagnose eye diseases is paramount for several compelling reasons, impacting public health, economic stability, and individual quality of life.
Preventing Irreversible Vision Loss: Many debilitating eye conditions, such as glaucoma and diabetic retinopathy, are progressive and often asymptomatic in their early stages. Early detection is absolutely critical to implement timely interventions that can prevent irreversible vision loss or slow disease progression. For instance, glaucoma can lead to permanent blindness if not managed, and diabetic retinopathy is the leading cause of blindness among working-age adults.
Reducing Healthcare Disparities: Access to specialized ophthalmologists and advanced diagnostic equipment is often limited in rural or underserved regions. This creates significant health inequities, where treatable conditions progress due to lack of screening. AI offers a scalable solution to extend diagnostic capabilities to primary care services and remote clinics.
Alleviating Clinician Burden: The rising prevalence of chronic diseases means an increasing demand for eye care. Ophthalmologists are often overwhelmed by patient volumes, leading to long waiting lists and potential diagnostic fatigue. AI can serve as an intelligent triage system, accurately identifying high-risk cases that require immediate specialist attention, thereby optimizing valuable human resources.
Economic Considerations: The societal and economic costs associated with vision impairment are staggering. This includes direct healthcare expenditures, lost productivity due to disability, and the burden on caregivers. Proactive screening and early treatment facilitated by AI can significantly reduce these long-term economic burdens by preserving vision and maintaining workforce participation.
Regulatory Compliance & Public Health: In some regions, there’s a growing emphasis on early detection programs for chronic diseases, including those affecting the eye. AI-powered screening tools can play a crucial role in meeting public health objectives by making systematic and widespread screening feasible, thereby improving population health outcomes and potentially influencing future healthcare policies.
2. Benefits of AI in Eye Disease Detection
AI-powered eye disease detection systems offer several compelling advantages over traditional methods, promising to transform ophthalmic care:
Objective Classification: Automated systems provide consistent, objective classification of retinal images, reducing inter-observer variability and human interpretation bias. This ensures a standardized and high-quality diagnostic baseline regardless of the clinician’s experience level or fatigue.
Scalability and Speed: AI systems can process thousands of retinal images in a fraction of the time it would take a human specialist. This capability is vital for large-scale screening programs, enabling rapid identification of individuals at risk and significantly reducing diagnostic backlogs.
Accessibility and Reach: AI models can be deployed in diverse settings, including remote clinics and primary care facilities where ophthalmologists may not be readily available. This expands access to critical eye care for populations in underserved areas, bridging significant healthcare disparities.
Data Analytics: AI systems facilitate historical tracking of disease progression and response to treatment. By analyzing large datasets over time, AI can identify emerging trends, predict disease trajectories, and inform more personalized treatment plans for individual patients.
Remote Monitoring: AI enables centralized monitoring of multiple patient populations across different geographical locations. This is particularly beneficial for managing chronic conditions like diabetic retinopathy, allowing for continuous oversight and timely intervention without the need for frequent in-person visits.
3. Data Preparation for Robust AI
Effective AI models are built upon robust and meticulously prepared datasets. The development of our eye disease detection model involved the aggregation and annotation of vast quantities of retinal images, captured under various operating conditions and environmental factors. Key characteristics of our dataset preparation include:
Balanced Representation: The dataset was curated to ensure a balanced representation of “normal” and “diseased” categories, including cataract, glaucoma, and diabetic retinopathy, to prevent model bias towards common conditions.
Image Capture Diversity: Images were captured using different fundus cameras, and at varying angles and distances, simulating real-world clinical scenarios and ensuring the model’s robustness to diverse imaging conditions.
Varied Illumination and Exposure: The dataset includes images captured under different illumination and exposure settings, further enhancing the model’s ability to generalize across various clinical environments.
Multiple Viewing Angles and Distances: Retinal images from various perspectives and zoom levels were incorporated to ensure the model could accurately interpret features regardless of subtle variations in capture.
High-Resolution Imagery: Utilization of high-resolution imagery was critical to capture minute pathological details, allowing the model to detect subtle indicators of disease that might be missed in lower-resolution scans.
Model Architecture
The foundation of our advanced eye disease detection system is the YOLOv9m architecture, a state-of-the-art object detection framework known for its speed and accuracy. We consistently provide SOTA models in every vision domain.
Key advantages of YOLOv9m in the context of eye disease detection include:
Real-Time Performance: Its optimized architecture allows for rapid inference, enabling near-instantaneous analysis of retinal scans, crucial for high-throughput screening environments.
Multi-Scale Feature Learning: Eye pathologies can appear at various sizes, from small microaneurysms in diabetic retinopathy to larger optic disc changes in glaucoma. YOLOv9m excels at detecting features across multiple scales.
Robust Feature Representation: The model’s sophisticated deep learning layers are highly effective at extracting intricate features from retinal images, capturing subtle biomarkers indicative of specific diseases.
Efficient Processing of Complex Patterns: Beyond static features, the model’s architecture enables it to efficiently process complex patterns and contextual information within the retinal image, leading to more nuanced and accurate diagnoses.
Training Parameters
The model was rigorously trained using the following configuration, optimizing for robust performance and reliable generalization:
Parameter |
Value |
Description |
|---|---|---|
Base Model |
YOLOv9m |
The foundational deep learning architecture employed for the task, known for its efficiency and accuracy in object detection. |
Batch Size |
8 |
Number of samples processed before the model’s internal parameters are updated, balancing training stability and computational efficiency. |
Learning Rate |
0.0005 |
Controls the step size during the optimization process, a conservative rate chosen for stable convergence and fine-tuning. |
Epochs |
70 |
Number of complete passes through the entire training dataset, ensuring the model learns extensively from the data and generalizes well. |
Optimizer |
AdamW |
An adaptive learning rate optimization algorithm (Adam with decoupled weight decay) known for its efficiency and strong performance in deep learning tasks. |
Inference Time |
~0.4s |
The average time taken for the trained model to process a single retinal image and output a diagnosis. |
Model Evaluation
Our rigorous training and validation processes have yielded a model with exceptional diagnostic capabilities, as evidenced by its strong performance across key evaluation metrics. Our model’s performance signifies a breakthrough in automated eye disease detection, proving its reliability for clinical application.
Metric |
Overall Performance |
Normal Eye |
Diseased Eye (Combined) |
|---|---|---|---|
Precision |
0.90 |
0.95 |
0.88 |
Recall |
0.94 |
0.97 |
0.92 |
F1 Score |
0.92 |
0.96 |
0.90 |
mAP |
0.95 |
0.96 |
0.93 |
Inference Time |
~0.4s |
- |
- |
Precision (0.90 Overall): This indicates that when our model identifies a disease, it is correct 90% of the time, minimizing false positives that could lead to unnecessary anxiety or follow-up.
Recall (0.94 Overall): With a recall of 94%, the model successfully identifies almost all actual disease cases, significantly reducing the risk of missed diagnoses (false negatives).
F1 Score (0.92 Overall): The F1 Score, a harmonic mean of precision and recall, provides a balanced measure of the model’s accuracy, reflecting its robustness in both identifying and correctly classifying conditions.
Mean Average Precision (mAP) (0.95 Overall): As a comprehensive metric for object detection and classification tasks, mAP of 0.95 signifies outstanding overall performance across all defined classes (cataract, glaucoma, diabetic retinopathy, and normal eye), indicating high accuracy and reliability.
Inference Time (~0.4s): The sub-second inference time ensures that diagnoses can be generated almost instantaneously, making it highly practical for clinical integration.
The per-category metrics further demonstrate the model’s reliability: “Normal Eye” detection shows slightly higher precision and recall, as healthy retina typically presents more consistent patterns. “Diseased Eye” represents an aggregated performance across the various pathologies (cataract, glaucoma, diabetic retinopathy), reflecting robust identification capabilities even for complex or subtle disease signs.
Epoch vs. Precision during Training
To demonstrate the training dynamics and performance stability of our model, the following graph illustrates the progression of precision over epochs. This visualization highlights how the model refined its accuracy during the training process, converging to a high level of precision.
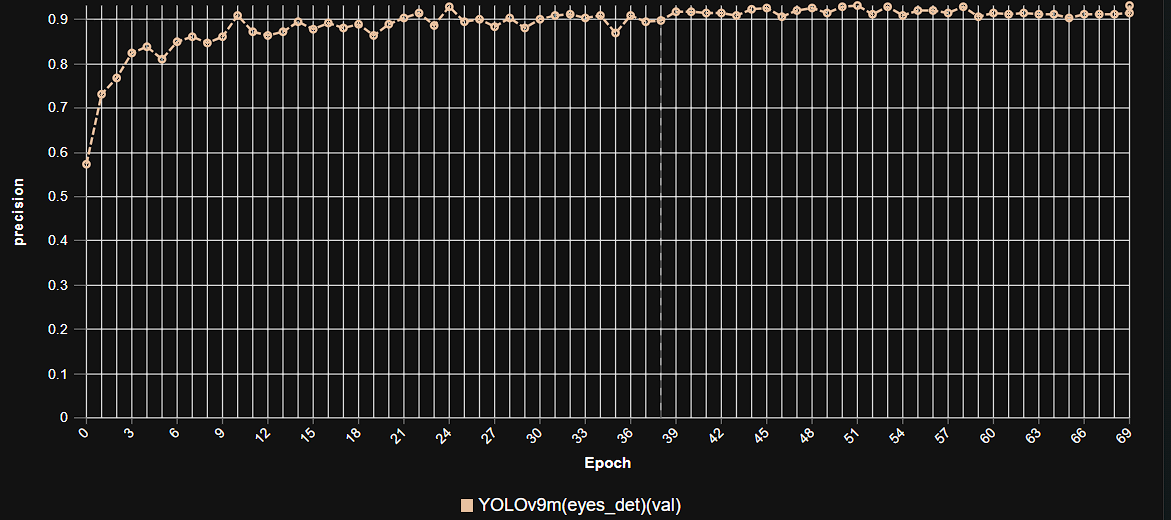 This graph illustrates the increase in model precision as training progresses over multiple epochs, showcasing the stable learning curve and high precision achieved by the YOLOv9m architecture in eye disease detection.
This graph illustrates the increase in model precision as training progresses over multiple epochs, showcasing the stable learning curve and high precision achieved by the YOLOv9m architecture in eye disease detection.
Model Inference Examples
Below are conceptual examples demonstrating the model’s output when processing retinal images for eye disease detection. The AI highlights regions of interest and provides classification, aiding clinicians in their diagnostic workflow.
Example 1: Detection of Diabetic Retinopathy
 This example illustrates our AI model accurately identifying and highlighting signs of diabetic retinopathy within a retinal image, demonstrating its capability for early disease detection.
This example illustrates our AI model accurately identifying and highlighting signs of diabetic retinopathy within a retinal image, demonstrating its capability for early disease detection.
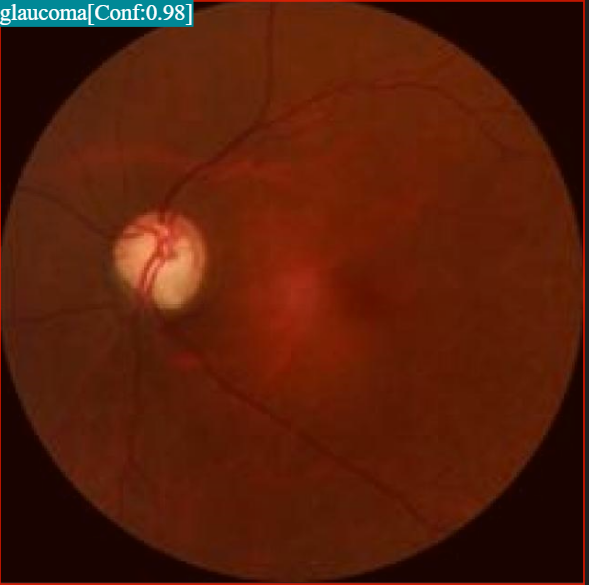
Example 2: Identification of Glaucomatous Optic Nerve Damage
 This image showcases the model’s ability to detect structural changes indicative of glaucoma in the optic nerve head, aiding in the diagnosis of this sight-threatening condition.
This image showcases the model’s ability to detect structural changes indicative of glaucoma in the optic nerve head, aiding in the diagnosis of this sight-threatening condition.
4. Real-World Applications and Impact
This AI-powered eye disease detection system has numerous real-world applications:
Telemedicine: AI enables remote diagnosis and consultation, bringing quality eye care to underserved areas.
Remote Clinics: AI-driven tools can serve as virtual assistants, helping general practitioners provide accurate referrals.
Mass Screening Programs: AI facilitates efficient and effective mass eye check-ups, identifying individuals who require further examination.
Primary Care Settings: AI screening tools can analyze retinal images for early signs of diseases, enabling earlier diagnosis and treatment even where patients may not have immediate access to an ophthalmologist.
5. Future Developments
Our commitment to innovation ensures continuous development and enhancement of our AI capabilities in ophthalmology. Future efforts will focus on:
Multi-Modal Data Integration: Expanding the model’s capabilities to integrate data from other ophthalmic imaging modalities, such as Optical Coherence Tomography (OCT) and OCT Angiography (OCTA), for a more comprehensive and robust diagnosis.
Explainable AI (XAI): Enhancing the interpretability of AI diagnoses by developing models that can not only classify but also highlight precisely why a particular diagnosis was made, fostering greater trust and clinical adoption among healthcare professionals.
Personalized Risk Assessment: Developing predictive models that can assess individual patient risk for disease progression or treatment response based on longitudinal data and genetic markers.
Edge Device Deployment: Optimizing models for deployment on mobile devices or portable imaging equipment, enabling on-site, instant diagnostic capabilities in even more remote or resource-limited settings.
Integration with Electronic Health Records (EHR): Seamlessly integrating AI diagnostic outputs into EHR systems to streamline clinical workflows, improve record-keeping, and support decision-making.
Conclusion
AI-powered eye disease detection represents a transformative leap forward in medical imaging and patient care. By delivering unparalleled accuracy, efficiency, and quantitative insights into ocular health, our solution empowers clinicians to make more precise diagnoses, plan more effective interventions, and ultimately improve outcomes for patients suffering from a wide range of eye conditions. As we continue to refine and expand these capabilities, the future promises an even more intelligent, data-driven, and compassionate approach to ophthalmic care.